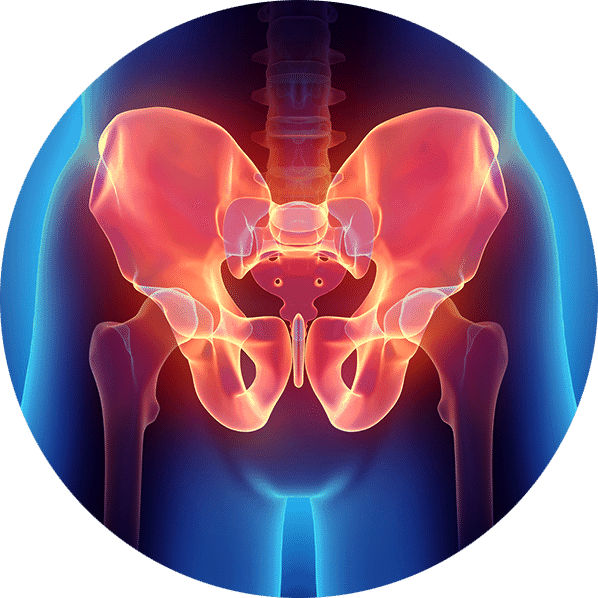
Chronic pelvic pain (CPP) often affects younger men (median age of 43) and is most often located at the perineal and genital regions but can manifest to other areas such as the lower abdomen, penis, scrotum, rectum, and lower back. The pain can initially come on suddenly with a duration that must be present for at least three of the last six months but can be characterised by continual remissions and relapses.
The pain often causes difficulties with bladder, bowel and sexual function. Pain on ejaculation is common and it can be difficult to urinate.
Most men with CPP will have their prostates ruled out as the cause of their pain. There is a growing body of research that shows a clear link between tension in the pelvic floor muscles causing pelvic pain. Normalising this pelvic muscle tension can have a huge impact on symptoms and your quality of life.